The skin and muscles frequently encounter injuries; while the skin forms a protective barrier against external insults, muscles can strain on stretching.1,2 Both tissues possess an elaborate repair program to effectively respond to and recover from injuries.
Tissue healing requires intricate synchronization between different cell types, particularly those of the immune and nervous systems, that act at distinct steps in the process to restore the tissue close to its original state.3 However, researchers were unaware of the exact extent of interaction between these cell types in tissue repair.
In a new study, scientists found that neuron endings grow into injured skin and muscle tissue and communicate with immune cells through a neuropeptide to promote tissue healing.4 These findings, published in Nature, provide insights on how neurons enable healing and open up potential therapeutic targets for regenerative tissue healing strategies.
“There are many different actors in the regeneration process,” said study author Mikaël Martino, a regenerative medicine scientist at Monash University and Osaka University. Although stem cells are the most commonly studied players, previous studies indicated crosstalk between the nervous and immune systems, which motivated Martino’s team to explore these following an injury.5
First, the team investigated how sensory neurons that detect pain, tissue injury, and inflammation modulate the immune system upon tissue damage. When they destroyed a subset of these cells in mice, they observed slower post-injury healing in their skin and muscles, whereas wounds of mice with intact sensory neurons healed within an expected timeframe.
The team next tracked sensory neurons to visualize their participation in tissue healing in mice. They observed that after injury, neuron endings grew in clusters around the damaged tissue, helping to innervate the area. The extent to which the sensory neuron endings grew into the damaged tissue was surprising, said Martino. “I was really excited to see, indeed, the nerve growing inside.”
Using immunofluorescence techniques, the scientists then discovered that the sensory neuron endings expressed a neuropeptide called calcitonin gene-related peptide (CGRP). This neuropeptide plays a role in wound healing and acts via the CGRP receptor complex on its target cells.6
To investigate whether CGRP modulated immune cell activity in injured tissues, the researchers generated mice whose immune cells lacked the receptor activity modifying protein 1 (RAMP1), a component of the CGRP receptor complex, rendering the cells unresponsive to CGRP. Upon wounding, these mice showed significantly impaired healing compared to wild type mice.
The team then profiled different cell populations during tissue healing using flow cytometry to gain insights into the immune players. They found that neutrophils, monocytes, and macrophages in injured mice with ablated sensory neurons behaved differently—the cells were present in higher numbers and showed more inflammatory characteristics—than those in mice with intact sensory neurons.
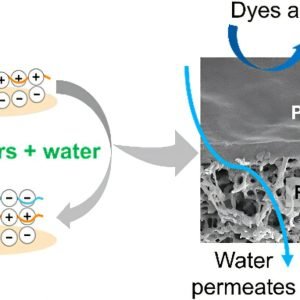
Neuron endings extend into tissues undergoing repair and influence immune cell function. A neuron ending cluster (red) surrounded by immune cells (yellow/orange) in an injured muscle.
Mikaël Martino and Yasmin Alshoubaki
Further investigations revealed that CGRP suppressed the recruitment of these cells to the injured tissue and accelerated their clearance after the cells had contributed to the initial phase of tissue healing. This helped reduce inflammation and shifted the damaged tissue toward a pro-repair state.
“What was really impressive about this study is it helped us understand the mechanism that neurons play in enabling healing,” said Yvon Woappi, a systems bioengineer at Columbia University, who was not involved with the study. Although he was not surprised that sensory neurons modulated the immune system during tissue repair, since these cells play key roles in inflammatory responses, Woappi noted, It’s elegant that someone was able to empirically demonstrate this by some very careful, rigorous experiments.”
In addition to studying the neuro-immune interaction, Martino’s team also explored its therapeutic potential. They tested the effect of purified engineered CGRP on skin and muscle injuries in mice with ablated sensory neurons and found that CGRP treatment promoted the closure of wounds even in the absence of sensory neurons. The treatment showed similar effects in diabetic mice that had damaged neurons in the body, or peripheral neuropathy. In these animals, CGRP improved wound closure and muscle regeneration compared to untreated mice.
“[This shows that] we probably can design new wound healing strategies for patients that have neuropathies by leveraging this neuro-immune interaction,” Martino said.
“It’s very encouraging to see such a dramatic effect on both skin and muscle healing in an animal model,” said Woappi, who, while enthusiastic about the findings, believes that the study lacks data on the applicability of the results to humans. “Although it’s an elegant study, well-performed in animal models, just a publicly available dataset of human tissue could have given some insight as to whether this mechanism is conserved in a human relevant context.” However, he believes it likely that a neuro-immune interaction may exist in humans since skin healing in rodents and humans is highly conserved.