A grumbling stomach provides the perfect cue that it is time to wrap up a meeting that is running into lunchtime and heavy eyelids are a clear sign that it’s time to sleep. The signals appear at appropriate times, thanks to the circadian clock. Using rhythmic environmental cues such as light, the circadian clock sets up a 24-hour internal oscillation that is replicated in every cell of the body.
The immune system is also regulated by the circadian rhythm.1 The body’s response to infections, vaccines, and even cancer is under circadian control. Now, a new study published in Cell shows that the efficacy of cancer immunotherapy is also dependent on the time of the day.2
Be it under healthy conditions or when the body is fighting a pathogenic invasion, white blood cells, or leukocytes, show oscillatory patterns. In mammals, the number of leukocytes in the blood peaks when the animal is resting; however, when it comes to leukocytes recruited to tissues, this pattern is reversed as it depends on the expression cycles of cell-surface proteins.3 These circadian immune rhythms also regulate antitumor immunity. Immune cells are more efficient in controlling the growth of tumors that are grafted into mice at specific times of the day and disrupting circadian rhythms leads to an increased risk of colon cancer in mice.4
“People had looked at oscillations in tumor cells and whether a tumor has a less robust circadian clock, but I wasn’t interested in the tumor cells themselves,” said Christoph Scheiermann, a circadian immunologist at the University of Geneva and a coauthor of the study. “For me, the more important thing was to investigate the host response.”
To understand how the host’s circadian rhythms contribute to tumor control, Scheiermann and his team injected mice with melanoma cells and, 12 days later, harvested the tumors at four different timepoints: one (T1), seven (T7), 13 (T13), and 19 hours (T19) after light onset. The latter two collection points occurred during the animal’s active phase. The researchers analyzed the number of tumor-infiltrating leukocytes (TILs) and found that they showed a time-dependent oscillatory pattern, peaking in the evening at T13, even though cells harvested at T19 had longer to proliferate. Rearing the mice in complete darkness throughout the day did not alter this rhythm, because, once established, circadian rhythms persist even if light is removed. However, reversing the light cycles, and thus the circadian clock, inverted the pattern of TILs, causing the cells to peak during the day.
To explore the contributions of the tumor microenvironment to the immune cells’ oscillations, the team used an antibody-mediated approach to block leukocytes from entering the tumor for 24 hours. This acute blockade reduced the TIL peak seen at T13 and nullified the time-of-day differences. Since TIL receptors are expressed on the endothelial cells in the tumor microenvironment, the team hypothesized that these cells could act as the gatekeepers at the blood-tumor border, timing the entry of TILs. Knocking out the circadian clock gene Bmal1—short for brain and muscle aryl hydrocarbon receptor nuclear translocator-like 1—in the tumor microenvironment endothelial cells caused the time-dependent TIL peaks to disappear.
“We were really surprised that the tumor kind of behaved like an oscillatory lymphoid organ,” Scheiermann said.
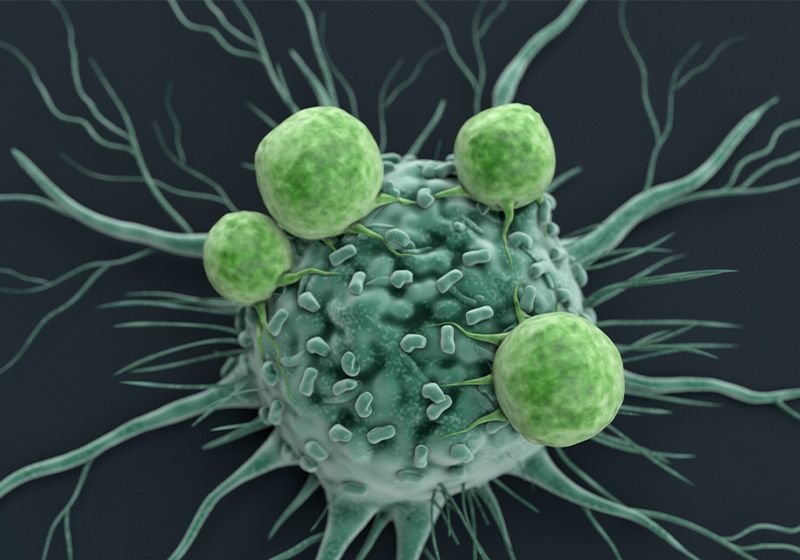
The team wanted to see if the complex oscillatory tumor-host interactions influenced the potency of anti-cancer therapies delivered at different times, essentially testing if chronotherapy helps kill tumor cells more effectively. Immunotherapy, one of the most promising treatments for tumors currently, makes use of the body’s built-in antitumor immune mechanisms.5 Two of the leading interventions, chimeric antigen receptor (CAR) T cells and immune checkpoint inhibitors, supercharge T cells to help them recognize and kill tumor cells. When the researchers administered CAR T cells or immune checkpoint inhibitors in the evening—the animal’s active phase—the therapies were more effective at controlling tumor growth than when they treated the mice during their inactive phase. Morning treatments had negligible effects on tumor growth. The enhanced effect of evening CAR T cell therapy vanished in mice that lacked Bmal1 in endothelial cells.
“What I loved about this work was that it shows that the timing of the first dose of the immunotherapy kind of sets the stage,” said Annie Curtis, a circadian immunologist at Royal College of Surgeons in Ireland University of Medicine and Health Sciences, who was not involved in the study. “From a clinical perspective, that’s very doable.”
Scheiermann noted that though immunotherapy given at any time will have some effect, giving it at the ‘wrong’, or less ideal, time will reduce its benefits dramatically. He added, “To see an effect, you will need to inject these antibodies at the right time.”
The authors also analyzed melanoma tumors removed from humans at different times of the day and found that TIL levels peaked in early afternoon, during the active window for most humans. Tumors from patients that responded to immune checkpoint inhibitors had an enrichment of genes similar to those in TILs extracted from mice at T13, indicating that timed immunotherapy can lead to better outcomes in cancer patients.
“I’m very excited about this because for me, it’s really the first time showing that chronotherapy works,” Scheiermann said. Going forward, the authors plan to delve deeper into why immunotherapies exhibit circadian effects despite their long half-life that spans multiple circadian cycles.
However, Curtis noted an important caveat. “This very nice time of day effect, do we just see this in people who have good, strong rhythms? Is this still there in individuals who are shift workers, elderly individuals?”






