The blood-brain barrier (BBB) regulates the passage of substances between the bloodstream and the brain, permitting essential nutrients and certain drugs to enter, while blocking harmful molecules.1 Disruptions to this critical function can lead to severe conditions like brain cancers and neurodegenerative disorders like Alzheimer’s disease.2 Despite its important physiological role in health and disease, scientist struggle to study this protective membrane, in part since the BBB of lab animals does not fully mimic the human BBB.3
“If we want to address BBB dysfunction, we have to have a good human BBB model,” said Ziyuan Guo, a neurobiologist and stem cell scientist at Cincinnati Children’s Hospital Medical Center.
Bridging this gap, Guo and his team developed brain organoids with a functional BBB that more closely mimics the organ in humans than previous mini-brain models.4 Their paper, published in Cell Stem Cell, describes a system that can help researchers study the BBB and investigate diseases associated with it.
“The whole approach of having organoids with a functional BBB is novel,” said Gad Vatine, a physiologist and cell biologist at Ben-Gurion University of the Negev, who was not associated with the study.
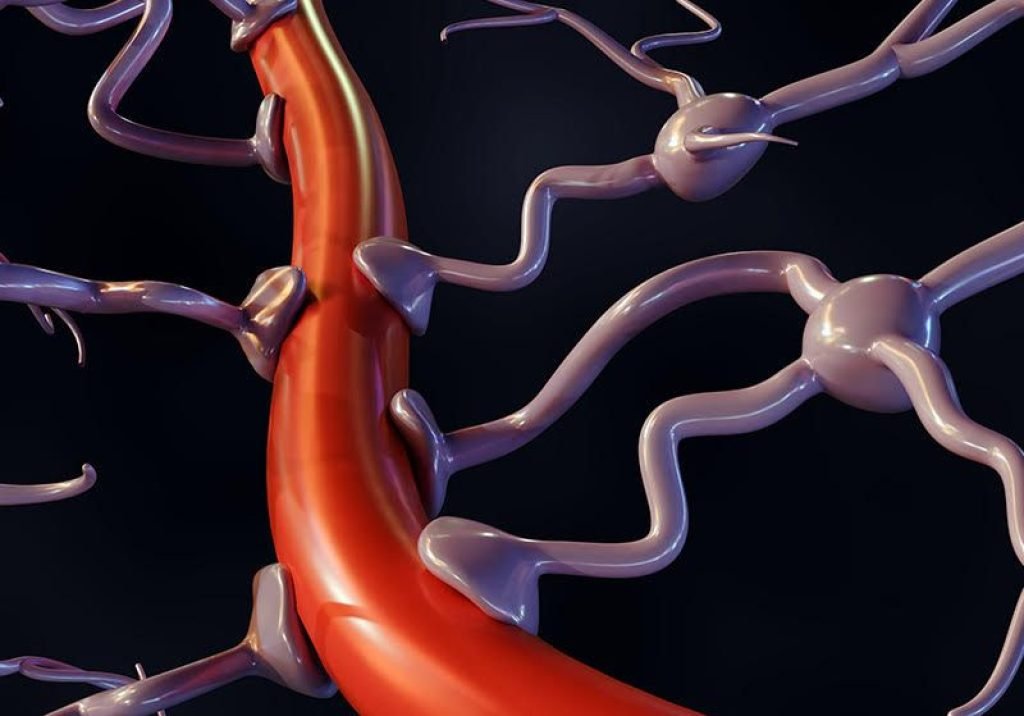
Designing BBB organoids posed a technical challenge: growing the two components—the brain and blood vessels—which arise from different germ layers during development, in the same dish. To overcome this hurdle, Guo’s team turned to established methods for growing brain organoids and blood vessel organoids using human pluripotent stem cells. After growing the cultures separately, they combined them to form assembloids, observing that the blood vessels grew into the brain tissue over the course of three weeks. The separate structures gradually fused to form a single sphere containing a network of capillaries.
Researchers combined blood vessel organoids (green, right) with brain organoids (dark green, left) to create an in vitro system for modeling the human blood-brain barrier.
Lan Dao, Ziyuan Guo
Immunofluorescence analyses of the assembloids revealed the expression of molecules like glucose transporters and tight junction proteins that are found in endothelial cells that line blood vessels in the BBB. In contrast, blood vessel organoids did not express these molecules before integrating into the cerebral organoids. To assess the barrier integrity of the assembloids, Guo and his team measured electrical impedance across the cells and observed high integrity, indicating that the structures mimic the organ’s barrier function.
To identify the cell populations in the assembloids, the researchers turned to RNA sequencing. This approach captured endothelial cells that line capillaries, neurons and supporting astrocytes, and other cell types associated with a functional human BBB. Unlike previous methods that only captured endothelial cells and neurons, the current approach produced nearly all the cell types of the neurovascular unit, noted Guo. He added, “So far, we are the ones most close to the real human BBB.”
Once they established that the assembloids resembled human BBB, the researchers explored whether they could use the system to model neurological diseases. They isolated stem cells from two patients with cerebral cavernous malformations (CCM), a genetic disorder marked by compromised BBB integrity, where clusters of thin-walled blood vessels can rupture and cause stroke.2
Using these patient-derived stem cells, they generated cerebral and blood vessel organoids. When merged to form assembloids, the structures replicated key features of CCM, including breakdown of the BBB. The patient-derived assembloids also showed characteristics similar to those observed in diseased biopsy tissue from patients with CCM.
The results were exciting, said Guo. He added, “This is a really big milestone in the field.”
Next, the team plans to use the assembloids to model other neurological conditions, such as autism spectrum disorder and Alzheimer’s disease.
Generating cerebral and blood vessel organoids and merging them together “is a breakthrough of the paper,” said Vatine. However, the researchers did not test whether substances can pass the BBB, he added.
“[The assembloids] still lack the technologies [to mimic blood flow] that will enable us to use them for prediction of what drugs will get into the brain,” he said. This is particularly important since preliminary drug testing relies on preclinical animal models, which do not completely capture what happens in humans, he explained.
Guo agreed that the assembloids need additional modifications. “We have to have a better improved model with the blood flow circulation which is the more accurate approach to measure drug [permeability],” he said. “But in terms of neurovascular interaction [between brain cells and blood vessel cells], we authentically mimic the real human BBB.”






