For decades, dogma dictated that the immune system consisted of two separate branches. Cells of the innate system respond rapidly to molecular patterns shared by a broad array of pathogens. Meanwhile, the adaptive system, consisting of T and B cells, responds more slowly, targeting specific antigens and generating long-lived memory cells to enable a quicker, stronger secondary response. But in recent years, the barrier between the branches has started to blur.
“More and more, it is more accepted that immunological memory can also be seen beyond adaptive immune cells,” said Itziar Martinez-Gonzalez, an immunologist at the Karolinska Institute. For example, both macrophages and natural killer cells display more rapid and robust secondary responses after initial stimulation, which Martinez-Gonzalez said is the key characteristic of immunological memory, regardless of the mechanism of activation.1,2
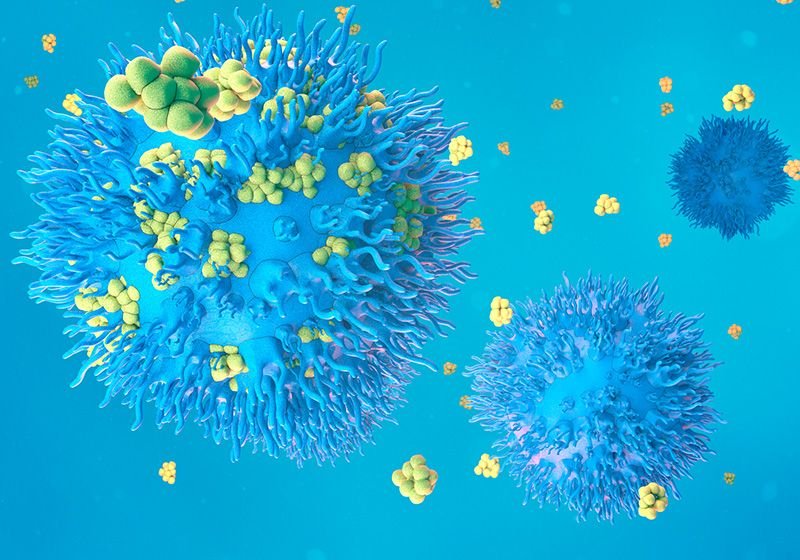
Itziar Martinez-Gonzalez and her team demonstrated that human tissues contained a population of ILC2s with memory-like abilities similar to their findings in mouse models.
Laura Mathä
As a postdoctoral fellow, Martinez-Gonzalez investigated the memory potential of another innate immune cell, type 2 innate lymphoid cells (ILC2s), which are activated by interleukin (IL)-33 and play an important role in the allergic response.3 Researchers dosed mice with IL-33 or an allergen to stimulate these cells, then, said Martinez-Gonzalez, “When we rechallenged these mice, ILC2s that were previously activated responded stronger and faster, so they were more sensitive.”
Martinez-Gonzalez was interested in determining if these memory ILC2s were present in humans as well. In a paper published in the Journal of Experimental Medicine, Martinez-Gonzalez and her group identified memory ILC2s in human tissues, expanding the field’s understanding of these cells and their contributions to immune responses and disease.4
The team began by studying two previous single-cell RNA sequencing data sets from patients with either asthma or atopic dermatitis.5,6 They observed a group of ILC2s that expressed less of a canonical ILC2 marker, IL-7 receptor (IL7R), but had increased expression of cytokines typically produced by ILC2s, such as IL4, IL5, and IL13.
The researchers sought to confirm these findings in new patient samples using flow cytometry. They found that in addition to reduced expression of CD127, the product of IL7R, these cells expressed CD45RO, a marker that identifies memory T cells. The researchers also found these CD127–CD45RO+ ILC2s in healthy individuals’ peripheral blood, skin, and intestinal samples, indicating that they can also be produced in response to everyday encounters with potential allergens.
To assess the functional aspects of the proposed memory ILC2s, the team isolated these cells and naive ILC2s and stimulated both populations with a cocktail of cytokines. Memory ILC2s produced more IL-5 and proliferated more than their naive counterparts, supporting their more robust recall response.
Finally, the researchers produced memory ILC2s in vitro. They isolated naive ILC2s and stimulated them with ILC2-activating cytokines or kept them in standard culture as a control for one week. Stimulated ILC2s proliferated rapidly over this time. Then, the team removed the activating cytokines and cultured the stimulated and non-stimulated ILC2s for one month to mimic a recovery period.
Most of the cells from the stimulated group died during the washout phase, leaving only a small cluster dominated by memory ILC2s. The team then treated both groups of cells with IL-33. The previously stimulated cells “remembered” this experience and responded more forcefully, producing more IL-5 and IL-13 than their naive counterparts.
“The paper does very good work in terms of dissecting specific activity and comparing and contrasting the memory population with [the] non-memory population,” said Rafeul Alam, an immunologist at National Jewish Health who was not involved with the study. He also said that the team’s investigation of ILC2s from multiple tissues made the conclusions more valuable, and that many of the genes and pathways they observed in humans echoed those found in mice.7
“It’s not as we thought at the beginning, that ILC2s only are important initiators of the inflammation, but then maybe we didn’t care about them when the disease was already chronic,” Martinez-Gonzalez explained. “Now it seems that, no, ILC2s can have roles during the chronic phases of the disease and respond even more strongly to different challenges.”
- Fang X-H, et al. Macrophage memory: Types, mechanisms, and its role in health and disease. Immunology. 2024;171(1):18-30.
- Cerwenka A, Lanier LL. Natural killer cell memory in infection, inflammation and cancer. Nat Rev Immunol. 2016;16(2):112-123.
- Martinez-Gonzalez I, et al. Allergen-experienced group 2 innate lymphoid cells acquire memory-like properties and enhance allergic lung inflammation. Immunity. 2016;45(1):198-208.
- Mathä L, et al. Human CD127 negative ILC2s show immunological memory. J Exp Med. 2024;221(8):e20231827.
- Ma J, et al. Single-cell analysis pinpoints distinct populations of cytotoxic CD4+ T cells and an IL-10+CD109+ TH2 cell population in nasal polyps. Sci Immunol. 2021;6(62): eabg6356.
- Alkon N, et al. Single-cell analysis reveals innate lymphoid cell lineage infidelity in atopic dermatitis. J Allergy Clin Immunol. 2022;149(2):624-639.
- Verma M, et al. NFκB1 inhibits memory formation and supports effector function of ILC2s in memory-driven asthma. Front Immunol. 2023;14:1217776.