For some diseases, a few vaccine doses enable lifetime immunity. But influenza requires annual vaccines to maintain immunity. One reason is because lung T cells only live for a few months. Understanding how to boost and maintain pathogen memory in the lungs would go a long way in bolstering protection against respiratory diseases.
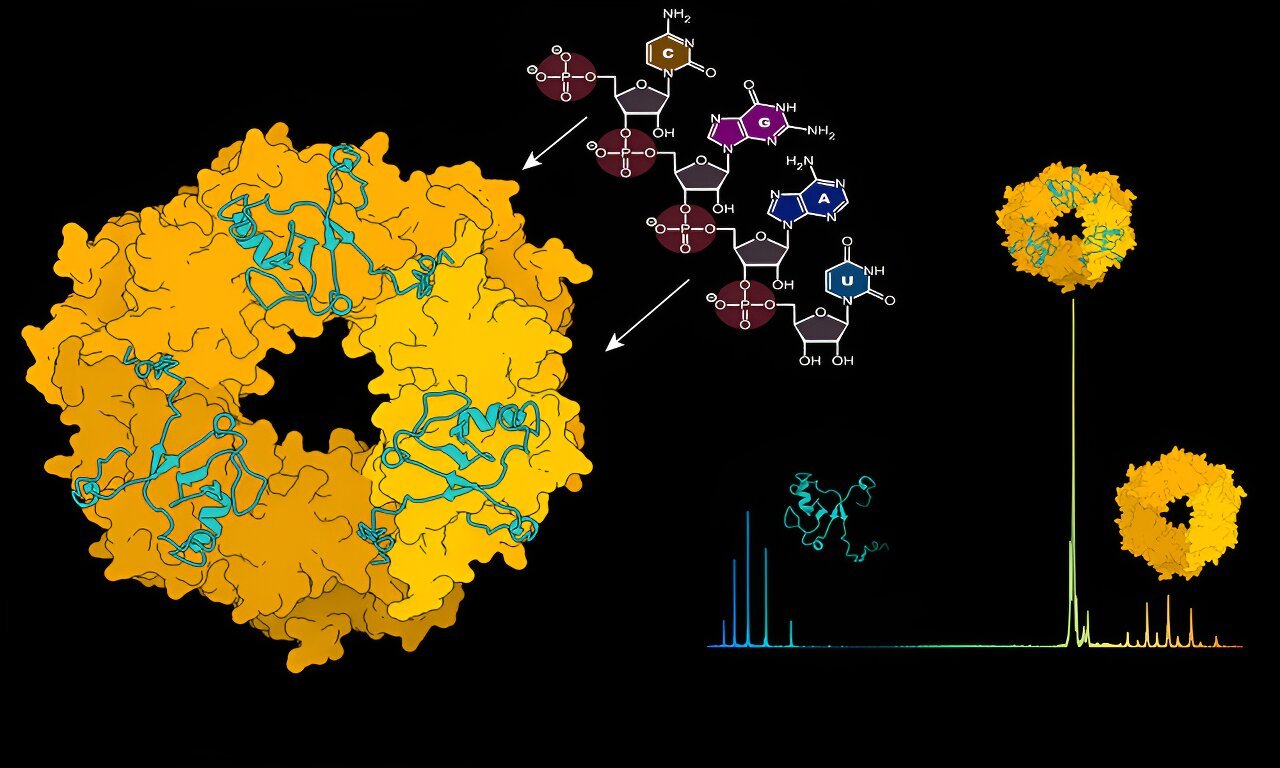
Recently, Emma Teixeiro-Pernas, an immunologist at the University of Missouri, and her team reported in the journal Nature Communications that the transcription factor, nuclear factor kappa B (NF-kB), which regulates immunity through a signaling pathway, can be tuned to maintain memory T cell populations in the lungs.1 Their findings pave the way for strategies that afford enhanced protection against subsequent infections.
In her previous studies, Teixeiro-Pernas found that modifying T cell receptor (TCR) signals in CD8+ T cells could help her understand how effector and memory T cells developed.2 In follow up studies, she found that the NF-kB signaling pathway, which TCR regulates, drives the generation and maintenance of memory T cells in response to an infection. This discovery prompted her to check if the function of the NF-kB signaling pathway was the same in every tissue, including the lungs.
To achieve this, the team engineered mouse models so that levels of NF-kB molecules could be regulated using the antibiotic doxycycline. They infected the mice with influenza virus, and after five days, they administered doxycycline for 25 days. Then they stained the blood vessels in the lungs to determine the number of lung resident memory T cells. Teixeiro-Pernas and her team found that when they fed the mice with doxycycline to increase NF-kB levels, the memory T cell population in the lungs dropped. The population, however, grew substantially when they blocked NF-kB expression. According to Teixeiro-Pernas, their findings indicate that NF-kB interferes with the generation of memory T cells in the lungs.
The next question on Teixeiro-Pernas’s mind was the timing of T cell decline. On tracing changes in the population size from the 10th day of infection with the influenza virus to the 30th day, the researchers observed that the number and frequency of T cell markers in the lungs started reducing 10 days postinfection and continued throughout the next 20 days.
Teixeiro-Pernas and her team were puzzled by this discovery because one of their previous studies had shown that once memory T cells were formed, their longevity depended on the level of NF-kB molecules.3 To clarify, they induced NF-kB signals in the mice 30 days after infection, after the memory T cells had formed. The team observed a four-fold increase in the population of memory T cells in the lungs. “What this is telling us is that the signaling pathway is critical for the generation of memory T cells, but it is not one way,” said Teixeiro-Pernas. “It depends on when in the immune response. This is important because it tells us when to intervene.”
“The way these things have been designed is very strategic,” said Stephen Jameson, an immunologist at the University of Minnesota who studies the regulation of memory T cells and was not involved in the study. He admired that the team refined old approaches to manipulate the signaling pathway and thus confirmed the assumption that the strength or duration of signals through T cell receptors determined the lifespan of memory T cells.
Teixeiro-Pernas believes that her findings have implications in cancer therapy and autoimmune diseases as tumors have low memory T cell loads, and immune cells are overproduced in autoimmune diseases.
According to Jameson, the study presents a different perspective for looking at memory T cells, but more work is needed before these findings could be applied therapeutically. “It’s good news that we have a way in which we can introduce more memory T cells at a vulnerable site in the lungs to give protective immunity. That could be a good thing. On the other hand, if there is too strong an inflammatory response, and you can no longer respire, then that is not good news,” he cautioned.
References
- Pritzl, C.J. et al. IKK2/NFkB signaling controls lung resident CD8+ T cell memory during influenza infection. Nat Commun 2023;14:4331.
- Teixeiro, E. et al. Different T Cell Receptor Signals Determine CD8+ Memory Versus Effector Development. Science 2009;323:502-505.
- Knudson, Karin M., et al. NFκB–Pim-1–Eomesodermin axis is critical for maintaining CD8 T-cell memory quality. PNAS. 2017;114(9):1659-1667.