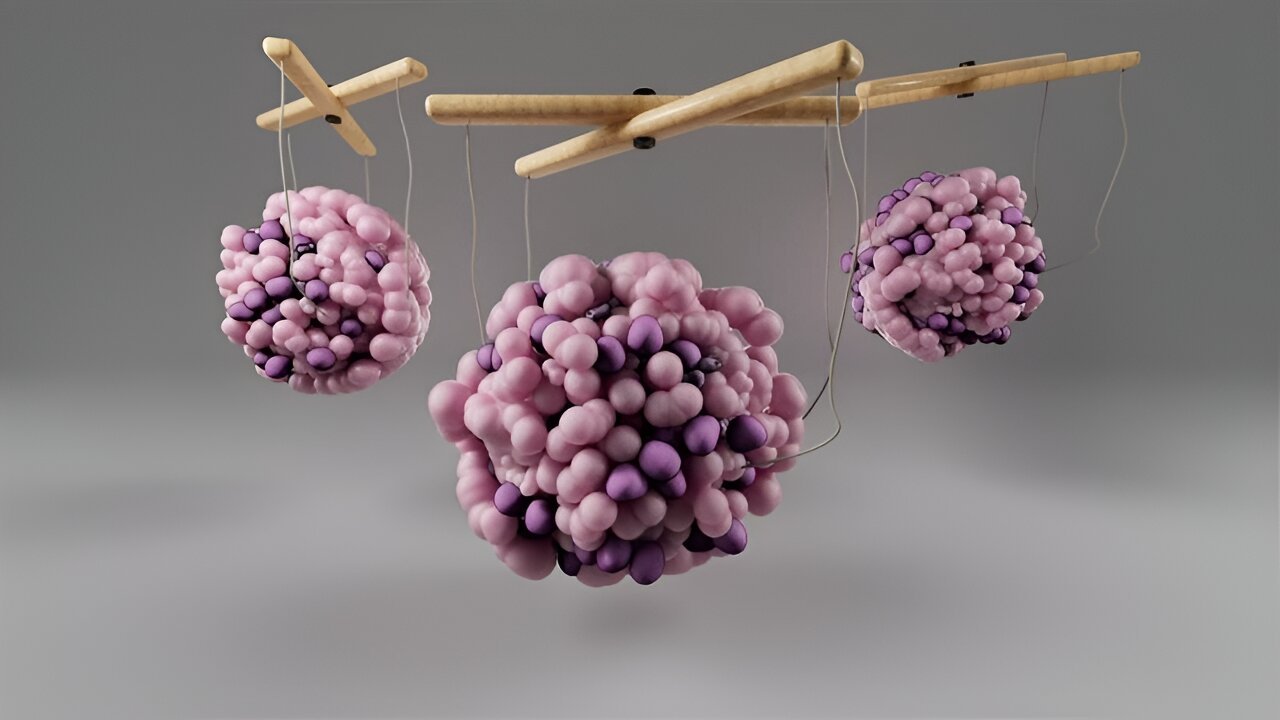
The cells in your pancreas, like people, can only handle so much stress before they start to break down. Certain stressors, such as inflammation and high blood sugar, contribute to the development of type 2 diabetes by overwhelming these cells.
Researchers at The Jackson Laboratory (JAX) have now discovered that DNA sequence changes known to increase a person’s risk for diabetes are linked to how well pancreatic cells can handle two different kinds of molecular stress. In people with these DNA changes, the insulin-producing cells in the pancreas may be more likely to fail or die when exposed to stress and inflammation.
“Ultimately, we want to develop new ways to prevent and treat type 2 diabetes by targeting the genes and pathways that are perturbed in people who are most susceptible to the disease,” said Michael L. Stitzel, associate professor at JAX and co-senior author with JAX professor Dugyu Ucar, of the study published in the Oct. 8 online issue of Cell Metabolism.
“These findings give us new insight into some of those genes and pathways.”
The work points toward dozens of genes that connect cell stress and diabetes risk, including one that is already under investigation as a drug target for type 2 diabetes complications.
Cells under stress
When living cells face challenges, including damage, inflammation, or nutrient changes, they activate protective responses to try to cope with and reverse the stress. But over time, sustained stress can overwhelm the cells, causing them to slow down or die.
In the pancreas’ islet beta cells, two types of cell stress have previously been implicated in the development of type 2 diabetes.
- Endoplasmic reticulum (ER) stress occurs when the cells become overwhelmed with a high demand to produce proteins—like insulin to help regulate blood sugar levels.
- Cytokine stress occurs when the immune system sends excessive inflammatory signals—as can occur in obesity and metabolic disease.
In both cases, the stress can eventually lead islet beta cells to stop producing insulin or die off.
Stitzel and his colleagues wanted to know what genes and proteins were used by islet cells to respond to both ER stress and cytokine stress.
“Researchers have completed multiple studies looking at what molecular pathways are important in regulating insulin production in happy, healthy islet cells,” said Stitzel. “But we were working on this hypothesis that islet cells are not always happy. So what pathways are important when the cells are under stress, and how do diabetes-linked DNA sequence changes in each of us affect them?”
Stress-response genes
Stitzel’s group exposed healthy human islet cells to chemical compounds known to induce either ER stress or cytokine stress. Then, they tracked changes to levels of RNA molecules in the cells as well as how tightly or loosely packed different stretches of DNA were inside the cells—a proxy for what genes and regulatory elements are being used by the cells at any given time.
To analyze the results, the team collaborated with Ucar, a professor and computational biologist at JAX . Together, the scientists found that more than 5,000 genes, or nearly a third of all the genes expressed by healthy islet cells, change their expression in response to ER stress or cytokine stress.
Many were involved in the production of proteins, which is crucial for islet cells’ insulin-producing role. And most of the genes were only involved in one or the other stress response, raising the idea that two separate stress pathways play a role in diabetes.
In addition, around one in eight regulatory regions of DNA typically used in islet cells were altered by stress. Importantly, 86 of these regulatory regions had been previously found to contain genetic variants in people most at risk of type 2 diabetes.
“What this suggests is that people with these genetic variants may have islet cells that respond worse to stress than other people,” said Stitzel. “Your environment—things like diabetes and obesity—pulls the trigger with type 2 diabetes, but your genetics loads the gun.”
Stitzel hopes that the new list of regulatory regions and genes will eventually lead to new drugs to prevent or treat diabetes by potentially making islet cells more resilient to stress.
A druggable target
The researchers homed in one gene that was altered by both stresses. Called MAP3K5, the gene was shown to alter islet beta cell death in mice containing a diabetes-causing mutation in the insulin-encoding gene.
In the paper, Stitzel and his colleagues showed that higher levels of MAP3K5 led to more islet beta cells dying in response to ER stress. Eliminating or blocking MAP3K5, on the other hand, made the islet cells more resilient to ER stress and less likely to die.
Early studies of Selonsertib, a drug targeting MAP3K5, have showed that it could reduce the risk of severe complications of diabetes. The new results point toward another possible role of the drug—in the prevention of diabetes in people most at risk of the disease, to help their islet cells remain functioning and alive in the face of cellular stress.
“It’s really exciting that this therapeutic is already in clinical trials but much more work is needed to understand whether the drug might be able to be leveraged in primary prevention,” said Stitzel.
More information:
Multi-omic Mapping of Human Pancreatic Islet Endoplasmic Reticulum and Cytokine Stress Responses Provides Type 2 Diabetes Genetic Insights, Cell Metabolism (2024). DOI: 10.1016/j.cmet.2024.09.006. www.cell.com/cell-metabolism/f … 1550-4131(24)00370-X
Citation:
How diabetes risk genes make cells less resilient to stress (2024, October 8)
retrieved 8 October 2024
from https://medicalxpress.com/news/2024-10-diabetes-genes-cells-resilient-stress.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.