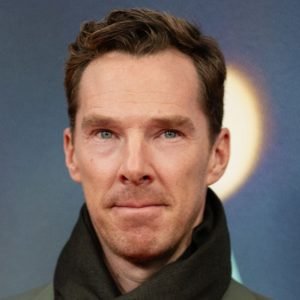
Whitty was “sceptical” about mandatory staff vaccination
Giving evidence to the UK Covid-19 Inquiry on 20 January,1 England’s chief medical officer, Chris Whitty, said that he had been personally sceptical about making covid vaccination a condition of employment for some healthcare staff in England. He said that the policy was “100% a political decision” that was essentially about balancing two risks and rights against one another: “the risk to the person who is being cared for versus the risk to the individual that their right to essentially not have a medical procedure, or lose their job, is protected.”
Whitty acknowledged a range of opinions on the issue, adding, “I’m rather more sceptical than some people that this is a good idea. But that’s a view as a citizen.” As a doctor, he argued that there was “a big difference” between a “professional responsibility” to protect patients from giving them communicable diseases, including vaccinating staff, and “legally mandating it so that you lose your job if not.”
NHS data sharing “has gone backwards” since pandemic
Whitty said he believed that NHS data sharing had “slipped backwards” since the pandemic. “We are now in a less good and more fragmented place than we were in the middle of the pandemic,” he told the inquiry. He said it was “regrettable” that changes to the “legal structure” during the pandemic, to allow data to be shared because there was an emergency, had now been reversed.
He highlighted the historical difficulty in, for example, linking up general practice and hospital data. “This is not good for patient treatment on an individual basis, and you can end up with someone going to several different settings and data that is held in one place is not held in another. That’s potentially dangerous,” he said. “We absolutely should be trying to . . . routinely join up data across the system, and then . . . if any emergency hits . . . that allows for a much more quick and effective understanding.”
Clinically vulnerable were let down, says former vaccine tsar
Kate Bingham, who led the government’s vaccine taskforce from May to December 2020, told the inquiry she believed that the lack of priority given to clinically vulnerable, immunocompromised people was “ethically and morally wrong.”2 When asked whether, during her time heading the taskforce, the issue of prophylactic development was left behind, she replied, “I absolutely felt that, yes, from late October 2020.”
By the time she left the post in December 2020, said Bingham, she was aware that the government would not be buying AstraZeneca’s Evusheld (tixagevimab-cilgavimab), a prophylactic antibody treatment. “I felt very strongly that we were conducting a strategy that was not following the prime minister’s goals,” she said, adding that it amounted to “a clear two tiered strategy where the clinically vulnerable immunocompromised patients were being deprioritised in favour of those who were able to receive vaccines.”
She added, “I felt that was manifestly wrong, both ethically and morally, but also, it did not follow the goals that we’d been set, which was to protect the entire population.”