Besides protecting heart health, widely used cardiovascular drugs could also significantly lower the risk of getting dementia in old age – by as much as 25 percent when used long term.
The findings come from a large study of 968,715 people, carried out by a team from the Karolinska Institute and Lund University in Sweden. The research looked at links between taking medications for at least five years, and the chance of developing dementia.
While the research doesn’t prove a casaul relationship between these drugs and dementia, it strongly suggests that a faulty heart might also open the door to cognitive decline – and perhaps that certain treatments can look after both the heart and the brain.
The link between cardiovascular health and dementia isn’t a new one, and studies have previously suggested that protecting the heart could also buffer against cognitive decline. However, so far the evidence to support that idea hasn’t been strong.
“Previous studies have focused on individual drugs and specific patient groups, but in this study, we take a broader approach,” says epidemiologist Alexandra Wennberg, from the Karolinska Institute.
The researchers looked at the impact of taking medication to manage hypertension, cholesterol levels, blood thinning, and fluids in the body (the diuretics that are often prescribed to treat heart failure).
These drugs were associated with a 4–25 percent lower risk of dementia, the data showed, and taking multiple medications typically had a greater effect in reducing risk than using a single drug on its own.
“We can see a clear link between long-term use – five years or more – of these drugs and reduced risk of dementia in older age,” says epidemiologist Mozhu Ding, from the Karolinska Institute.
However, another type of heart medication had the opposite effect.
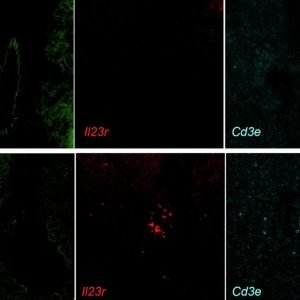
Antiplatelet drugs, which stop platelets in the blood from clumping together and triggering strokes, were associated with a 13–25 percent increase in dementia risk – possibly because the anti-clumping effect makes brain microbleeds more likely, the researchers suggest.
In addition, short-term use of any of the cardiovascular drugs studied was linked to a 13–30 percent increase in dementia risk – which may be down to the medication being started too late in life to have a protective effect on cognition.
A possible reason for the increase is that heart conditions may raise dementia risk. Some medications, like those for high blood pressure, are also given for early cognitive decline symptoms, making the connection harder to understand.
Each of these associations will need to be investigated further before conclusions are drawn.
The researchers did discuss some of the biological mechanisms that might be protecting both hearts and minds – such as the benefits of cholesterol reduction across the body – but they’re keen to point out there are many other factors in play, including diet and exercise, which could be explored in future trials.
“We currently have no cure for dementia, so it’s important to find preventive measures,” says Wennberg.
The research has been published in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association.