Colorectal cancers, which kill more than 900,000 people each year, are notoriously heterogeneous. The cell type and the genetic mutations that give rise to the tumors and the effect of the tumor microenvironment on their growth can vary widely. This diversity can lead to incorrect characterization of the tumors, ultimately resulting in less-than-ideal treatment plans.
Colorectal tumors start off as pre-cancerous masses called adenomas that form in the mucosal lining of the large intestine. This lining renews itself every three to four days to compensate for the daily wear and tear it suffers.1 When this regenerative cycle goes haywire, cancer develops.2 Until recently, scientists thought that the two types of adenomas—conventional and serrated—grew from different cell types in the intestinal lining. This lining contains U-shaped pockets, or crypts, with intestinal stem cells (ISCs) at the base and differentiated cells at the top. The prevailing theory stated that conventional adenomas grew from stem cells at the base of the crypt, while serrated adenomas arose from abnormal cells at the top. Researchers and clinicians termed these the bottom-up and top-down models and have designed preventive and therapeutic strategies based on these categories.3 Now, a new study published in Developmental Cell has overturned this theory by showing that conventional and serrated adenomas grow only after ISCs are lost and two distinct populations of multipotent stem cells appear at the bottom and top of the crypt, revival stem cells and fetal-metaplasia cells, respectively.4 These precancerous cells divide to form adenomas, making both tumor types bottom-up.
“The study looks at an important area of colorectal cancer biology using rigorous mouse models. And it’s attempting to address two pathways by which colon cancer initiates,” said Nilay Sethi, a cancer biologist at the Dana-Farber Cancer Institute who was not involved in the study. Sethi emphasized the need for studies like this one that shed light on the molecular details of how serrated adenomas form and progress to hard-to-treat tumors. Identifying potential targets for treatment can help clinicians tackle this aggressive cancer more effectively.
“If we don’t understand how a tumor starts, we will not be able to prevent it,” said Maria Diaz-Meco, a cancer biologist at Weill Cornell Medicine and coauthor of the paper.
Previous studies from the authors revealed that loss of two atypical protein kinase C (aPKC) isoforms, PKCλ/ι and PKCζ, resulted in the growth of serrated adenomas in the intestines of mice.5 These proteins regulate the differentiation and death of intestinal cells. “We discovered that two atypical protein kinase C [isoforms] are reduced in colorectal cancer, particularly in those patients that have a worse prognosis,” said Jorge Moscat, a cancer biologist at Weill Cornell Medicine and coauthor of the paper. He emphasized that the expression levels of genes encoding these proteins could help identify the severity of the disease in these patients. Counterintuitively, intestinal cells from mice lacking aPKC or only PKCλ/ι fail to form viable organoids. The team wanted to understand the reason for this discrepancy and the events leading up to the formation of the adenoma. They created mice that lacked aPKC in the epithelial cells of the intestines and observed how that affected the stem cells. Deletion of aPKC in the epithelium not only led to the formation of serrated tumors, but these tumors had lost all their ISCs and instead had metaplastic cells of different identities. The loss of ISCs also explained why these mutant intestinal cells could not multiply to grow organoids.
“The loss of the stem cells following this loss of the kinases was most surprising to me. I don’t necessarily think about normal stem cells dying when colon cancer is starting,” Sethi commented.
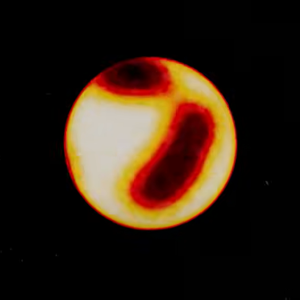
Stem cell loss driven by aPKCs deficiency precedes the formation of colorectal adenocarcinomas. The image shows a healthy intestinal lining (left panel) and a precancerous adenoma progressing to form a cancerous tumor (second panel onward).
Anxo Martinez-Ordoñez, Weill Cornell Medicine
To understand the sequence of these early events, the researchers did a timed deletion of one or both aPKC in intestinal epithelial cells, including stem cells, of mice. Deleting both PKCλ/ι and PKCζ caused a strong reduction in the stem cell population three days after the deletion compared to wild type mice. This was followed by the appearance of precancerous cells at the top and bottom of the crypt. Deleting only PKCλ/ι was sufficient to reproduce the same chain of events. The team also observed that aPKC deletion led to the activation of cell death transcription programs in the stem cells. The resulting loss of ISCs caused the entire crypt structure to crumble, followed by the appearance of precancerous cells that can divide uncontrollably to produce adenomas starting from the top or the bottom. Through these experiments, the team showed that aPKCs play a crucial role in maintaining ISCs. Loss of these cells triggers a chain reaction that ends in a tumor.
The effects of aPKC loss in mice were mirrored in humans. The team procured samples of conventional adenomas and serrated adenomas from human patients and analyzed the levels of aPKC in them. All of the serrated adenomas and 71 percent of the conventional adenomas had reduced levels of aPKC as compared to healthy tissue. Staining the different cell types in these tumors showed that all the serrated adenomas and 90 percent of the aPKC-deficient conventional adenomas were devoid of ISCs.
“We never expected the stem cells to be lost. It was well established in the field that stem cells were the cause of cancer. So, it was very paradoxical why these cells die,” Diaz-Meco said.
The team also investigated what happens in advanced cancerous tumors; they observed a strong correlation between the loss of both aPKCs proteins and tumor development.
“Our dream is to put aPKC on the map,” Diaz-Meco said. She envisions a future where colorectal tumors are screened for levels of aPKC, to design the best therapy for each patient.
Though the study showcases the importance of aPKC in the initiation of colorectal cancers, questions remain about how and when mutations in the aPKC genes arise.